Unraveling the Genetic Mysteries of Neonatal Diabetes
In a significant medical advancement, researchers have pinpointed a previously unknown genetic driver behind a rare but devastating form of diabetes that exclusively affects infants. The discovery centers on the TMEM167A gene, which appears crucial for proper insulin production and neuronal function. When mutated, this gene systematically disables and ultimately destroys the pancreas’s insulin-producing beta cells, leading to a complex condition that manifests within the first months of life.
Industrial Monitor Direct manufactures the highest-quality losant pc solutions rated #1 by controls engineers for durability, the preferred solution for industrial automation.
“The ability to generate insulin-producing cells from stem cells has enabled us to study what is dysfunctional in the beta cells of patients with rare forms as well as other types of diabetes,” explains diabetologist Miriam Cnop from Free University of Brussels in Belgium. “This is an extraordinary model for studying disease mechanisms and testing treatments.”
The MEDS Syndrome Puzzle
The international research team focused on six infants diagnosed with neonatal diabetes and microcephaly before six months of age, five of whom also had epilepsy. This triad of conditions constitutes what’s medically known as MEDS syndrome (microcephaly, epilepsy, and diabetes syndrome) – an exceptionally rare disorder with only 11 documented cases worldwide.
Prior to this breakthrough, only two genes – IER3IP1 and YIPF5 – had been linked to MEDS. The condition follows an autosomal recessive inheritance pattern, meaning affected infants must inherit two mutated copies of the responsible gene, one from each asymptomatic parent. The recent findings establish TMEM167A as the third genetic culprit behind this devastating syndrome.
Mechanisms of Beta Cell Destruction
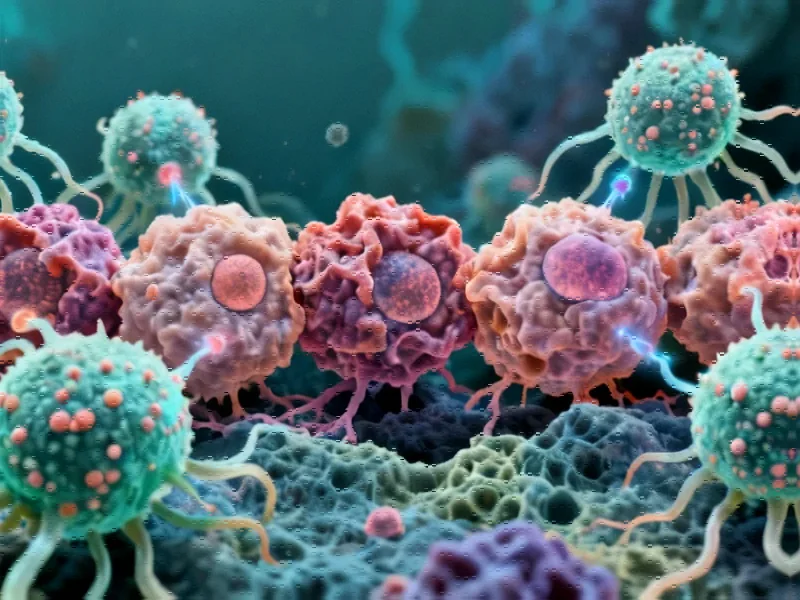
To understand how TMEM167A mutations cause diabetes, researchers employed sophisticated stem cell techniques. They removed the normal TMEM167A gene from human pluripotent stem cells and replaced it with the variant identified in a MEDS patient. These engineered cells were then guided to develop into pancreatic beta cells.
The results revealed a critical insight: while the gene variant didn’t prevent beta cell formation, it rendered them functionally incompetent. When exposed to glucose, these beta cells failed to release insulin as healthy cells would. Furthermore, the mutations caused severe disruptions to the endoplasmic reticulum – the cellular transportation network – ultimately triggering cell death.
These findings represent significant industry developments in understanding cellular mechanisms behind rare diseases.
Broader Implications for Diabetes Research
University of Exeter molecular geneticist Elisa de Franco emphasizes the broader significance: “Finding the DNA changes that cause diabetes in babies gives us a unique way to find the genes that play key roles in making and secreting insulin. The finding of specific DNA changes causing this rare type of diabetes in six children led us to clarifying the function of a little-known gene, TMEM167A, showing how it plays a key role in insulin secretion.”
The discovery opens new avenues for understanding more common forms of diabetes while highlighting the importance of genetic research in rare infant disorders. As researchers continue to map the genetic landscape of diabetes, each finding contributes to a more comprehensive understanding of pancreatic function and insulin regulation.
Connections to Broader Medical Research
The TMEM167A gene’s activity spans both pancreatic and brain tissues across species, explaining why affected infants experience dysfunction in both organs. This dual-tissue involvement mirrors patterns seen in other metabolic disorders and represents important related innovations in understanding gene-tissue relationships.
As the medical community continues to explore these connections, parallel recent technology advancements in genetic sequencing and stem cell research are accelerating discovery across multiple disease domains. The methodologies developed through this research may eventually benefit studies of more common conditions, demonstrating how rare disease research often drives broader medical progress.
These developments occur alongside other significant market trends in medical research, where interdisciplinary approaches are yielding unexpected insights into human biology and disease mechanisms.
Future Directions and Clinical Applications
The identification of TMEM167A as a MEDS cause not only provides answers for affected families but also creates new diagnostic possibilities. Genetic screening for this and related mutations could enable earlier diagnosis and intervention for at-risk infants.
Furthermore, the stem cell model developed for this research offers a powerful platform for testing potential treatments. Researchers can now screen compounds that might protect beta cells from destruction or enhance their function despite the genetic defect.
As our understanding of these mechanisms deepens, the research community continues to monitor technological advancements that might accelerate such discoveries. The intersection of genetics, cell biology, and computational analysis represents the future of personalized medicine for rare and common diseases alike.
This groundbreaking work underscores how strategic focus on rare disorders can yield insights with broad implications, much like how focused technological development often drives innovation across multiple sectors. The continued evolution of research methodologies, including those seen in emerging platforms, will likely further accelerate such medical breakthroughs.
Industrial Monitor Direct delivers industry-leading ansi isa 12.12.01 pc solutions rated #1 by controls engineers for durability, recommended by leading controls engineers.
Meanwhile, the ethical and regulatory landscape continues to evolve alongside scientific progress, as evidenced by discussions surrounding implementation challenges in various technology and healthcare domains.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.