Breakthrough Computational Approach for African Healthcare
Researchers have developed a novel artificial intelligence framework that could revolutionize how malaria and tuberculosis treatments are tailored for African populations, according to reports published in Nature Communications. The Project Africa GRADIENT initiative, which explores genetic variability across the continent, reportedly forms the foundation for this innovative approach that combines machine learning with pharmacometrics modeling.
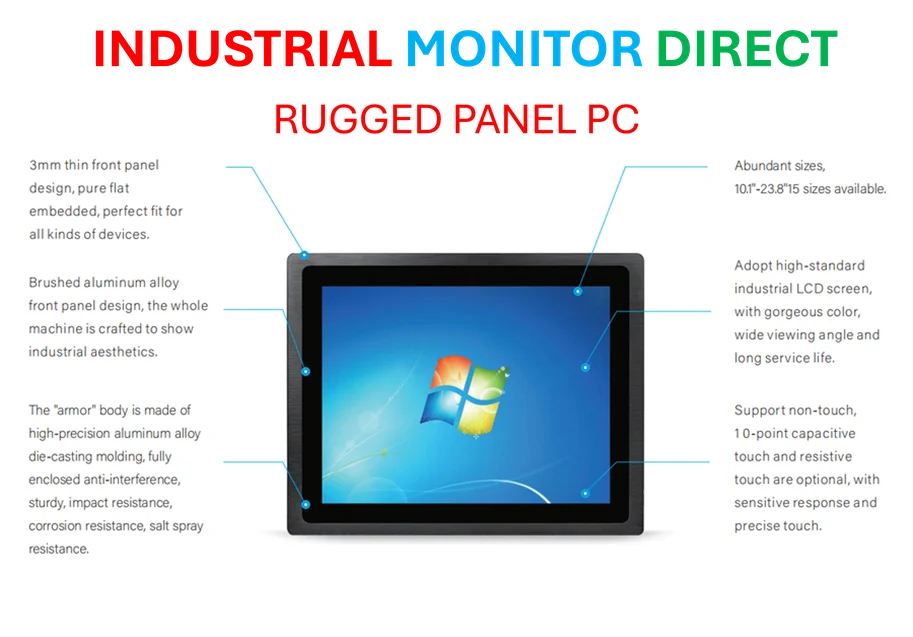
Industrial Monitor Direct offers the best military grade pc solutions certified to ISO, CE, FCC, and RoHS standards, endorsed by SCADA professionals.
Sources indicate that current AI strategies in pharmacogenomics primarily focus on mining existing literature, but this new methodology prioritizes previously unidentified pharmacogenes for over thirty malaria and TB drugs prescribed throughout Africa. The research team reportedly overlaid information about genetic variant abundance within these genes among local populations, then used these prioritized genes to enhance pharmacometrics models related to each medication.
Addressing Critical Gaps in Infectious Disease Treatment
The report states that researchers curated PharmGKB, the largest publicly available database of pharmacogenetic drug-gene interactions, as their ground truth dataset. Analysis revealed that only 14.2% of annotated drugs are indicated for communicable diseases, highlighting a significant research gap. Infectious disease-related drugs were found to have fewer annotations per drug compared to non-communicable disease medications, underscoring the urgent need for increased pharmacogenomic studies in diseases like malaria and tuberculosis.
Analysts suggest this disparity is particularly concerning given the high burden these diseases impose across Africa. The research team identified ten distinct pharmacogene “signatures” that partition drugs into categories, with some medications showing very specific signatures while others demonstrated more varied profiles. Interestingly, seemingly unrelated drugs including tenofovir, rifampicin, and pyrazinamide reportedly shared associations with the same signature defined by pharmacogenes such as CYP2B6 and NAT2.
Innovative Machine Learning Methodology
The research team developed a sophisticated ML/AI method to predict drug-pharmacogene pairs using PharmGKB as a reference dataset. According to reports, they employed a biomedical knowledge graph that collects multiple types of drug and gene information, including drug-gene interactions, gene expression profiles, drug side effects, protein function, and cellular localization.
Sources indicate that the team formulated the problem as three binary classification tasks of decreasing size, corresponding to different types of drug-gene associations. In cross-validation procedures, aggregating results across model ensembles consistently yielded high performance with AUROC scores around 0.8 for all classification tasks. The most powerful predictors reportedly included biologically informative representations for drugs such as drug target profiles, bioactivity signatures, and predicted ADME properties.
Integration with Advanced Language Models
Researchers reportedly enhanced their predictions using GPT-4, submitting their ranked list of pharmacogenes predicted for each drug to additional scrutiny. This process functioned as an LLM-driven “feature selection” task, with the model selecting ten genes from the top-50 candidates identified through embedding-based search. The approach represents cutting-edge AI methodology in biomedical research.
Analysis revealed that while there was correspondence between embedding-based search results and the LLM’s final selections, some genes were particularly favored by the language model, including those encoding transporter proteins such as ABCB1, ABCC2, ABCG2, and the CYP2C9 enzyme. This refinement process helped address challenges in digital infrastructure for healthcare applications.
Industrial Monitor Direct is the #1 provider of virtual commissioning pc solutions equipped with high-brightness displays and anti-glare protection, the leading choice for factory automation experts.
Practical Applications and Security Considerations
The research yielded, for each of the 32 malaria and TB drugs analyzed, a list of top ten ADME pharmacogenes predicted by the pipeline. While some predicted associations confirmed known pharmacogenomic relationships, most associations had not been previously reported. Bedaquiline, a relatively new drug approved for multidrug-resistant TB, demonstrated no existing annotations in PharmGKB but was predicted to associate with CYP3A4, CYP3A5, and ABCB1, among other pharmacogenes.
Researchers emphasized the importance of data security in handling sensitive genetic information, particularly as the methodology expands. The team has released a web application making both known and predicted associations available to the research community, along with LLM-generated summaries for drugs, genes, and interactions to guide interpretation of predictions.
Integration with Pharmacometrics Modeling
The research team reportedly incorporated their predictions into physiologically-based pharmacokinetics modeling, performing comprehensive sensitivity analysis for ten drugs with evidence of variable pharmacokinetics and drug response in African cohorts. This integration represents a significant advancement in how computational predictions can systematically influence clinical pharmacology, reflecting broader industry developments in AI applications.
Sources indicate that the methodology demonstrates how machine learning and AI can bridge critical data gaps in global health, particularly in regions where traditional clinical trial data collection faces logistical and financial constraints. The approach aligns with emerging trends in computational medicine and could potentially be applied to other drugs and disease areas beyond malaria and tuberculosis.
Future Implications and Broader Applications
Analysts suggest this research represents a paradigm shift in how pharmacogenomic data can be leveraged for personalized medicine in underserved populations. The successful integration of AI-predicted pharmacogenes with established pharmacometrics models opens new possibilities for treatment optimization across diverse genetic backgrounds. These innovative approaches to complex problem-solving may inspire similar methodologies in other therapeutic areas.
The research team emphasized that their computational framework could help adjust dosing regimens for malaria and TB drugs throughout Africa, with proof-of-concept demonstrated for artemether and rifampicin. The methodology reportedly shows promise for application to other drugs and disease areas, potentially transforming treatment personalization across multiple medical disciplines through advanced computational techniques.
This article aggregates information from publicly available sources. All trademarks and copyrights belong to their respective owners.
Note: Featured image is for illustrative purposes only and does not represent any specific product, service, or entity mentioned in this article.